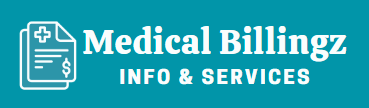
If your health sector employs medical billing regularly, you might have encountered claim denials in some of the applications. That of course results in revenue loss and a lack of motivation to operate efficiently. In order to get every claim approved by the government or private organization, there is a strategy called AR recovery. That you can implement in medical billing and prevent revenue decline.
What Is AR Recovery?
RCM cycle starts when a patient gets a health treatment and ends with receiving reimbursement and obtaining patient bills on time.
But if some bills are not paid or claims are not fulfilled, what procedure supervises these situations? AR recovery process is what helps hospitals keep a regular follow-up on claims.
AR in term AR recovery stands for “Accounts Receivable”. It helps recover that revenue that would have been lost due to claim denial, rejection, and late response.
Many insurance companies show a slow response towards making reimbursement, that leads to diminished revenue. The lengthier the claim approval process, the least chance you have of getting your reimbursement.
However, with the help of AR recovery follow-ups, you will be able to get the revenue that might have lost if you didn’t take a step to receiving it.
Importance Of AR Follow-Ups
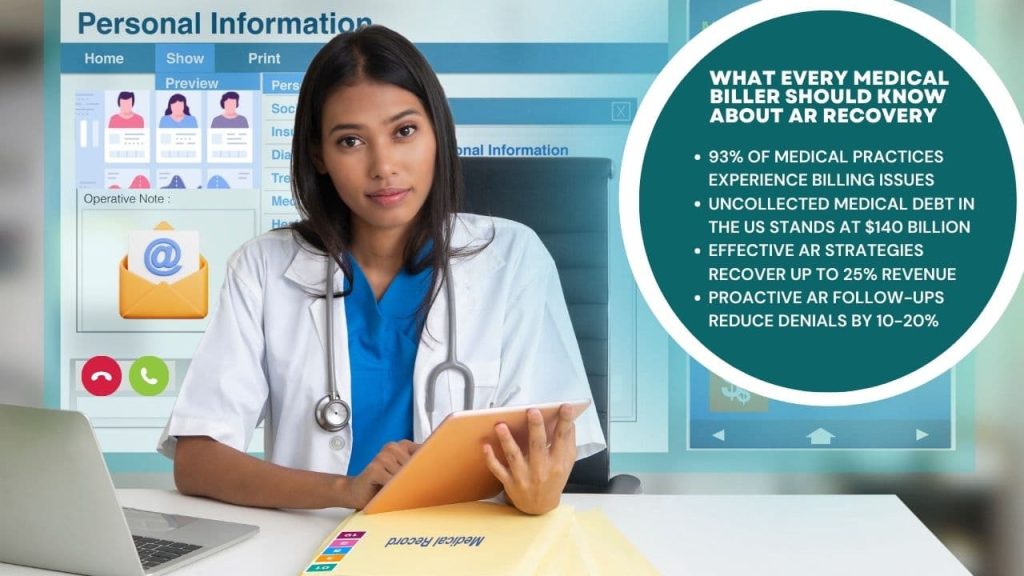
Every single claim application contains its duration. That means each claim application has a certain time span to be paid. This process is conducted by classifying similar-level claim applications with an aging report.
These reports are monitored continuously to focus on those that are still not paid.
If any of the claims has exceeded its age, denial management and the AR recovery team work together to get the payment. Their team analyzes pending claims and identifies the cause of denial. Then they work to resolve the problem and get the payment.
Following is the impact of AR recovery on healthcare facility’s financial health:
| Financial Metric | Description | Impact of Effective AR Recovery |
| Cash Flow | Movement of cash into and out of the business | Improved cash flow with timely payments |
| Revenue Cycle | Total time taken from providing service to receiving payment | Shortened revenue cycle |
| Bad Debt Rate | Percentage of uncollectible accounts | Reduced bad debt with better collection practices |
| Operational Costs | Costs associated with managing AR | Lower costs due to efficiency improvements |
| Patient Satisfaction | Patient’s experience with billing and payments | Higher satisfaction with clear communication and options |
Secondly, denial management teams and AR recovery staff re-submit denied claims after solving the problem. After which they keep checking the status of queued and denied claims and make sure the claim is paid in full.
How AR Recovery Be Helpful In Medical Billing

As you have seen the importance of the AR recovery process, now you must understand how these procedures help hospitals get revenue. Here are some ways this strategy can help you get revenue without disrupting the reimbursement process.
Keep A Track On The Application
Proper and regular tracking enables you to monitor the progress of claim applications. It acts as a reporting system that shows what are the improvements that need to be made in order to receive revenue.
With the help of this, you can make the operation efficient by solving any problem that arises during the medical billing process.
Set Clear Goals
AR strategy involves setting up clear goals and objectives. Not only does this keep you following the right way, but it also helps you measure the metrics you want to focus on in RCM.
These following metrics will also help you exhibit better performance in the future and avoid recovery mistakes.
| Metric | Description | Ideal Value |
| Collection Rate | Percentage of revenue collected | > 95% |
| Days in AR | Average days to collect receivables | < 40 days |
| Denial Rate | Percentage of claims denied | < 5% |
| Write-Off Rate | Percentage of uncollected claims written off | < 3% |
| Follow-Up Rate | Percentage of claims followed up within set time | 100% |
| Net Collection Rate | Net revenue collected compared to net charges | > 95% |
| Gross Collection Rate | Total revenue collected compared to total charges | > 90% |
| First-Pass Resolution Rate | Percentage of claims resolved on first submission | > 85% |
| Appeals Success Rate | Percentage of denied claims successfully appealed | > 50% |
| Average Payment Lag | Average time between claim submission and payment | < 30 days |
| Patient Payment Rate | Percentage of patient payments collected on time | > 95% |
| AR Aging Distribution | Breakdown of AR by age (e.g., 0-30, 31-60 days) | < 20% over 90 days |
| Percentage of Claims Under Follow-Up | Percentage of total claims currently being followed up | < 10% |
| Cash Acceleration Rate | Improvement in cash flow from AR efforts | Positive growth |
| Bad Debt Recovery Rate | Percentage of previously written-off debt recovered | > 10% |
| Patient Satisfaction Rate | Percentage of patients satisfied with billing process | > 90% |
| Cost to Collect | Expenses incurred in collecting receivables | < 5% of total collections |
| Revenue per Full-Time Employee (FTE) | Amount of revenue collected per billing staff member | Increasing trend |
| AR Turnover Ratio | Frequency with which AR is collected and replaced | > 8 times per year |
Follow-Up
After claim submissions, recovery plan keeps you updated about the claim status. It promptly notices any claim rejection and its reason.
AR strategy also enables the submission of claim appeals after resolving the payer rejection.
Proven Strategies For Successful Recovery
No healthcare facility would want to lose their revenue by knowing they deserve that. For this, they implement a number of tactics to ensure revenue collection.
However, in terms of AR recovery, when implementing the process, let us tell you some tips that will maximize the impact of your efforts and guarantee ample revenue collection.
Timely And Accurate Documentation
Meticulous documentation is the cornerstone of an effective recovery.
Make sure that all patient data, rendered services, and insurance information are timely and properly recorded. This speeds up the billing procedure and decreases the potential of mistakes that might cause delayed payments.
Verify Insurance Information
It’s critical to confirm and double-check the patient’s insurance information before starting any billing procedures. Verify the specifics of the policy, the limits of the coverage, and any requirements for submitting claims.
This proactive step accelerates the reimbursement process and helps avoid denials.
Clear Communication With Patients
Have open lines of communication with patients about their financial obligations. Explain co-pays, deductibles, and any unpaid balances in detail.
By giving this information up front, you will reduce surprises and improve the chance that payments will be made on time.
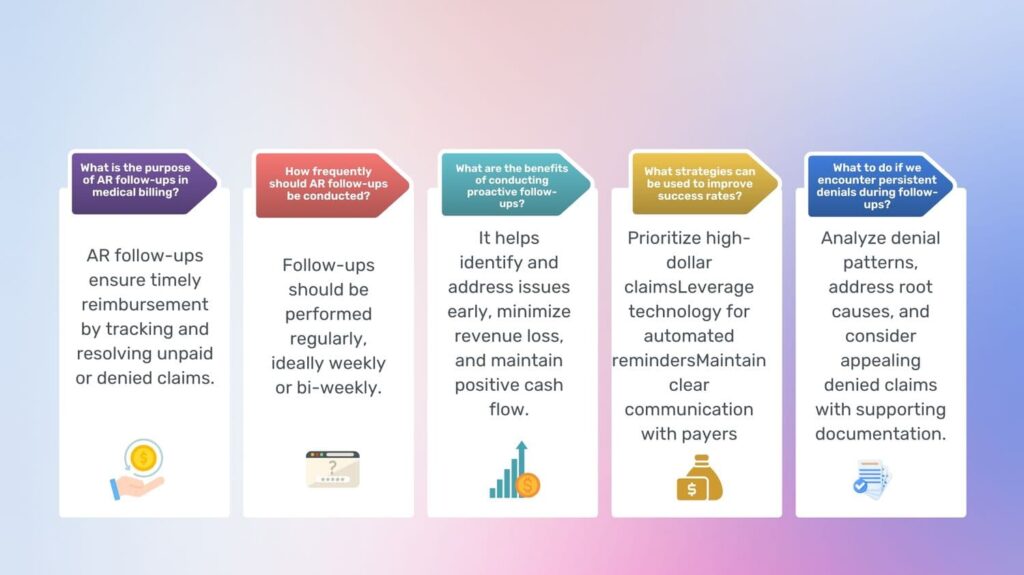
Conduct Effective Denial Management Using Our Tips
Automate Billing Processes
Use technology to automate the billing process. This covers automated follow-ups, electronic claim submissions, and patient and insurer reminders.
Automation speeds up the entire process and lowers manual error.
Regularly Monitor And Analysis
Establish a system for routinely observing and evaluating AR data. Monitor maturing accounts and look for any trends or patterns of claim rejection.
By taking a proactive stance, problems can be quickly addressed before they worsen. It eventually leads to faster recovery rates.
Appeal Denied Claims
Have a methodical process for resolving claims that are rejected. Recognize the reasons for the denial, gather the required paperwork, and file as soon as possible.
AR recovery can be considerably improved by perseverance and having a deep understanding of the appeals procedure.
Utilize Advanced Technologies
Investigate and incorporate cutting-edge technologies like predictive modeling and analytics powered by AI. These tools can be used to anticipate payment patterns, spot possible problems with the AR process, and improve collection tactics.
Staff Training And Education
Make an ongoing training investment for your billing staff.
Keeping them informed about the most recent rules governing the industry, changes in coding, and best practices guarantees a more competent and effective team, which eventually raises the rates of successful recovery.
Challenges Associated With Recovery Process
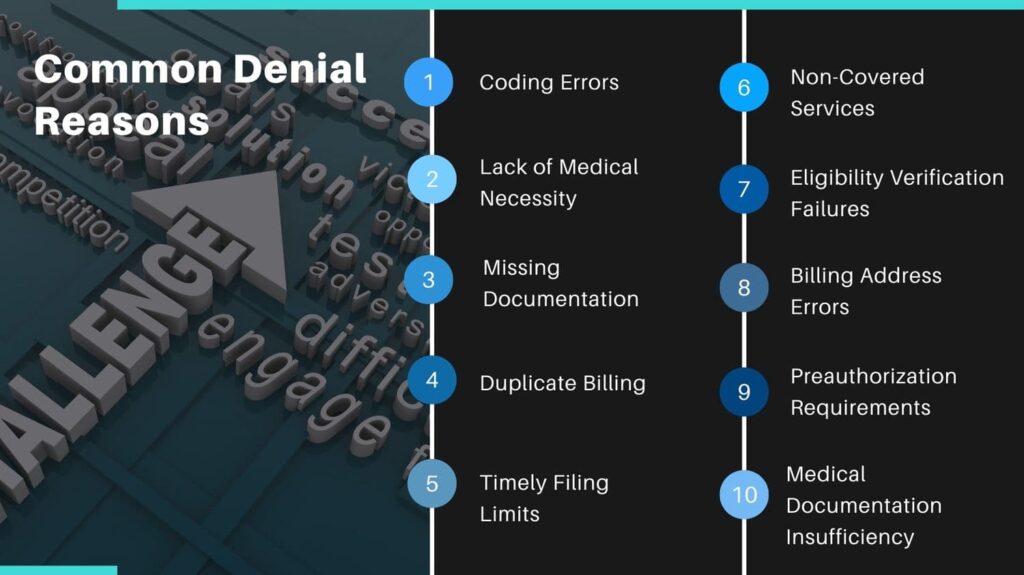
There are a few challenges of AR recovery that are threatening the RCM cycle of hospitals. Here are some of them and solutions to avoid it:
Payment On Time
Patients tend to pay more late than insurance organizations. This is because a heavy medical bill becomes difficult for them to pay. But to get your revenue, you must first make sure to send accurate bills.
Besides, to get timely payments you must also provide multiple payment options to the patients. This way they can better respond according to their preferred method.
Additionally, provide terms of additional charges on only late payments. This will make patients pay their bills on time to avoid extra fees.
Offer Multiple Payment Plans
Patients are more likely to respond quickly if they are provided with multiple modes of payment, especially through credit cards. Offer various suitable credit and payment plans to help patients choose the best one.
Even during debt collection practices, when the patient is already suffering from debts, you can offer multiple payment plans to make them pay on time instead of showing a late response.
Yearning to explore how to manage claim denials? Set forth by clicking the button.
Maintain A Positive Patient Relationship
When patients are paying their bills through any of the provided payment methods, maintain a positive attitude towards them to appreciate their involvement.
Send daily reminders to let them know the achieved milestone and remaining installment. It is also a good idea if you offer discounts to the patients when the bill is paid on time.
AR Management
Any mistake during the AR recovery process may result in complete revenue loss.
To overcome this you must automate the process in order to efficiently conduct AR and save your time. For this, you can use a number of automated and end-to-end AR systems to manage the process systematically.
Besides, automated systems offer you a great opportunity to handle all the tasks through a single platform. That means a more streamlined process that will help you get your revenue much easier.
Miscommunication
Sometimes, a lack of proper communication may lead to confusion. Which in turn, results in late payments and responses by the patients. However, you must make sure to maintain a productive communication means with patients through online portals.
Answer their queries and resolve any problems they have been facing.
Furthermore, keep updating your policy page with the latest guidelines and payment addresses to help patients know about the payment process.
Get Your Revenue!
All of the points mentioned above prove the significance of implementing AR processes in medical billing. We have also listed some of the challenges associated with the process, that might help you if you are new to AR recovery.
Even if you are an experienced user of the process, these challenges may help you predict the future and tailor your services accordingly.
In the end, if followed responsibly, AR recovery can yield positive results and provide you with maximized revenue.