By enabling smooth data interchange between systems, Electronic Data Interchange (EDI) has completely transformed a number of industries. EDI is a vital component of medical billing in the healthcare industry, enhancing transaction speed, accuracy, and efficiency.
What is EDI?
The electronic exchange of data using standardized formats between various organizations is known as electronic data interchange, or EDI. Paper-based techniques are replaced by this technology, allowing for faster and more accurate data exchange.
The Function of EDI in Medical Billing Streamlining Billing Processes:
EDI streamlines billing information exchanged between payers and healthcare providers, reducing errors and speeding up payment cycles.
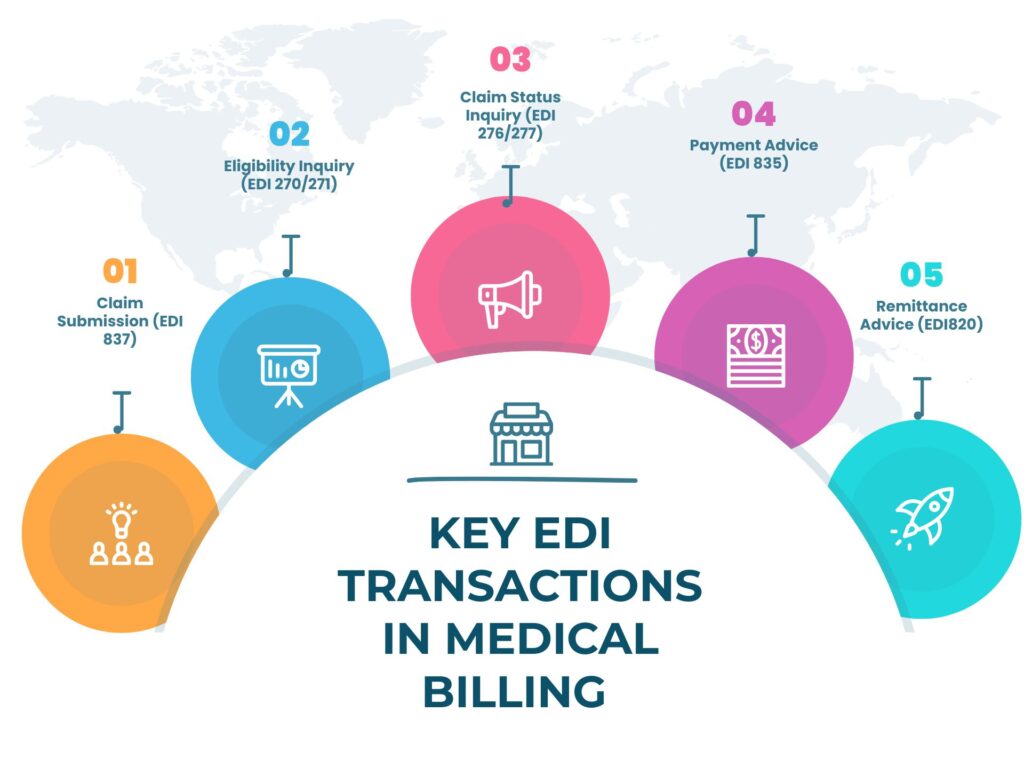
Common Transactions of EDI in Medical Billing:
Claim Submission (EDI 837): This is the process by which healthcare providers submit claims for services rendered to insurance payers. Eligibility Inquiry and Response (EDI 270/271): This transaction verifies patient eligibility and benefits information.
Claim Status Inquiry and Response (EDI 276/277): This is used to find out the status of submitted claims. Payment and Remittance Advice (EDI 835): Provides information about insurance company payments and any adjustments made to the billed amount.
Advantages of EDI in medical billing
Sensitive patient data is safeguarded during transmission thanks to strict security protocols and encryption in EDI billing. Few of the advantages are enlisted below:
Enhanced Effectiveness
Human error is minimized when data exchange is automated by reducing the need for manual data entry. This effectiveness results in shorter processing times and less administrative work.
Savings on Costs
Costs related to paper-based billing, such as printing, shipping, and storage charges, are greatly reduced by using EDI. It also lowers labor expenses associated with processing claims manually.
Enhanced Precision
Accurate and consistent data are guaranteed by automated procedures and standardized formats. This expedites the reimbursement process and lowers the possibility of claim rejections brought on by mistakes.
The Medical Billing Industry’s EDI Process
- Healthcare providers compile the relevant EDI billing data as part of data preparation.
- EDI software is used to translate information into EDI format.
- Through a secure network, the formatted data is sent to the payer.
- The payer certifies that they have received the data.
- Following the claim’s processing, the payer replies.
- After money is transferred, the supplier receives a remittance advice.
Standards and Software for EDI in Medical Billing
Healthcare organizations can handle the complete EDI process with the aid of a variety of EDI software options. These software programs ease data interchange and guarantee adherence to industry standards.
Guidelines in EDI
Healthcare EDI standards such as ANSI X12 specify formats and protocols for various kinds of transactions.
HIPAA Compliance: Maintains patient confidentiality and protects health information by making sure that all EDI transactions adhere to the Health Insurance Portability and Accountability Act (HIPAA).
| EDI Transaction | Description |
| 837 Professional | Submits healthcare claim information to insurers. |
| 837 Institutional | Sends claim data for inpatient and outpatient services. |
| 835 Remittance Advice | Details payments and adjustments made by insurers. |
| 270/271 Eligibility | Checks patient eligibility and insurance coverage. |
| 276/277 Claim Status | Inquires and responds to claim status updates. |
The Difficulties of Using EDI in Medical Billing
Initial Expenses of Setup
An EDI system’s setup expenses, including software and training, can be substantial. However, long-term savings and increased efficiency usually outweigh these expenses.
System Integration It can be difficult to integrate EDI with the current healthcare administration systems. Careful planning and coordination between IT and medical professionals are needed.
Technical Difficulties
Challenges can arise from technical problems like data mapping, translation errors, and network connectivity. For smooth operation, regular updates and maintenance are required.
Adherence to Regulations
It’s difficult to stay on top of legal changes and make sure standards like HIPAA are followed. A violation of the law may lead to fines and legal problems.
The Value of EDI in Health Care Billing
Healthcare personnel are not burdened with as much administrative work when billing processes are automated through EDI. Staff members can concentrate on more value-added activities, like patient care and strategic planning, by cutting down on manual tasks.
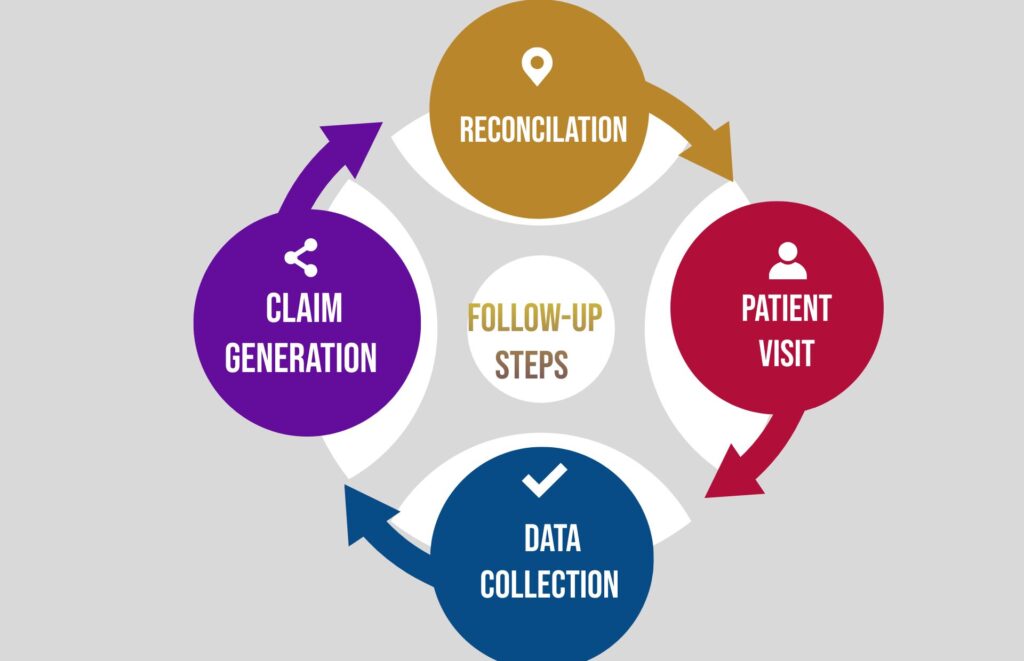
EDI in medical billing streamlines the entire billing process.
Raising the Rate of Reimbursement
Enhancing accuracy and expediting processing, EDI in medical billing contributes to a higher percentage of successfully processed reimbursements. In the end, timely and accurate claims submission improve revenue cycle management by reducing delays and denials.
Increasing Patient Contentment
Patients have fewer problems with billing when paperwork is processed more quickly and accurately, which makes for a better overall experience. Patients are happier with their healthcare services overall when there are fewer billing disputes and clearer statements.
Assisting with audits and compliance
EDI systems make it easier to comply with regulations and streamline audit procedures. Healthcare providers will be able to effortlessly prove compliance in audits and inspections thanks to their ability to generate comprehensive records and reports.
Encouraging Data Integration
Electronic data interchange EDI in medical billing facilitates the smooth integration of billing data with other healthcare systems, including practice management and electronic health records (EHR). The accuracy and consistency of billing data across various platforms is guaranteed by this integration.
Making Scalability Possible
EDI systems are scalable, meaning they can accommodate higher transaction volumes as healthcare organizations expand. Because of their scalability, billing procedures can grow with the company without compromising their effectiveness.
EDI’s Problems and Solutions for Medical Billing:
Complex Integration Issues
It can be difficult to integrate EDI systems with current billing and Electronic Health Records (EHR) systems. Ensuring seamless communication between these disparate systems is a significant challenge, as healthcare organizations frequently use a variety of software systems.
Healthcare providers can work with seasoned EDI billing service providers who provide strong integration solutions to tackle integration problems. Enabling middleware to function as an intermediary between EDI billing systems and EHR billing systems can improve data flow.
Prior to a full-scale implementation, comprehensive system assessments and pilot testing can also assist in identifying and resolving integration issues.
Data Protection and Adherence
Challenge: Since the medical field handles extremely private patient data, data security is crucial. EDI transactions have to abide by rules like the U.S. Health Insurance Portability and Accountability Act (HIPAA), which requires strict data protection procedures.
Solution: To secure sensitive data during EDI billing, use advanced encryption protocols and secure communication channels. To make sure that regulatory requirements are being followed, regular security audits and compliance checks are crucial. Risks can also be reduced by regularly updating security systems and educating employees on best practices for data security.
Problems with Standardization
EDI standards used in the healthcare sector, like ANSI X12 and EDIFACT, can be complicated and differ between various organizations. To prevent mistakes and delays in transactions, it is essential that all parties use compatible standards.
Standardized formats and protocols must be used for all EDI transactions. To guarantee adherence to pertinent standards, healthcare organizations and their EDI service providers should collaborate closely.
To minimize inconsistencies and simplify transactions, trading partners should have open lines of communication and agree on standard formats and procedures.
Does EDI speed up insurance reimbursements?
Expense of Implementation
Especially for smaller healthcare providers, the upfront costs of implementing EDI systems can be significant. These expenses cover hiring new employees, integrating the system, and purchasing software.
Healthcare companies can begin with a phased implementation strategy to control costs. To test EDI capabilities, start with a pilot program and progressively grow it based on the outcomes. Numerous EDI in medical billing service providers provide scalable solutions that enable incremental investments and grow with the company. Using cloud-based EDI solutions can also offer flexibility and lower upfront costs.
In summary
The introduction of automation and standardization through Electronic Data Interchange (EDI) has brought about a significant transformation in healthcare transactions, improving efficiency, accuracy, and cost-effectiveness.
The use of EDI in medical billing procedures has improved data security and regulatory compliance while streamlining administrative tasks, lowering manual errors, and quickening the reimbursement cycle.
Important lessons learned:
EDI in medical billing streamlines and automates the billing process, allowing for quicker payments and claim submissions. Reduced administrative workload and improved cash flow are the results of this efficiency.
Standardized EDI formats reduce the possibility of human error in manual billing, which lowers the number of claim denials and increases billing accuracy.
HIPAA and other regulations are complied with and sensitive patient data is safeguarded through the use of encryption and strict security standards in EDI transactions.

EDI in medical billing lowers printing, mailing, and storage expenses by doing away with the need for paper-based procedures. Furthermore, it lowers the costs related to rework and claim rejections.
EDI billing systems help support regulatory compliance and better financial management by providing comprehensive reporting and analytics capabilities.
Essentially, EDI in medical billing is a fundamental component of contemporary healthcare transactions, promoting enhancements in healthcare organizations’ overall financial stability, accuracy, and efficiency. Its advantages go beyond merely streamlining operations; it also helps to improve patient satisfaction and budgetary control.
The use of EDI in medical billing is anticipated to increase as technology develops, incorporating cutting-edge technologies like blockchain, artificial intelligence, and cloud computing to maximize its efficacy.
In a nutshell, adopting EDI in medical billing is a smart move that promotes the long-term viability and prosperity of healthcare providers in addition to being a technological advancement.
Through the utilization of EDI in medical billing, healthcare institutions can optimize their processes, enhance their financial outcomes, and ultimately provide superior patient care.
FAQs
How is medical billing efficiency increased through EDI?
By streamlining the billing and payment procedures, eliminating errors, decreasing the need for manual entry, and automating data exchange, EDI increases efficiency.
Is it safe to send medical billing data using EDI?
EDI is secure, yes. In order to ensure compliance with HIPAA and other regulations, it employs encryption and other security measures to protect sensitive healthcare data during transmission.
What role does EDI play in regulatory compliance?
By following the standardized formats and protocols mandated by healthcare laws like HIPAA, EDI ensures that all data exchanges comply with industry and legal standards, thereby aiding in compliance.

