Smooth revenue generation during RCM revenue cycle management is a dream of many hospitals, but only some of them become successful in achieving those ambitions.
The reason is that these health facilities stay one step ahead in making their RCM superior.
In order to excel in revenue generation, health practices make sure they follow some quality checks, that help them keep their services under those standards that reward them in extensive revenue generation.
Ignite Your RCM Knowledge — Click Now to Unlock a World of Insights.
Let’s have a look at these standards, that you too can follow and be one of those health facilities that don’t let their revenue run away.
Why It Is Important To Maintain RCM Quality?
Suppose you have hundreds of claims in a day to deal with, all of them can collectively provide financial stability to your health facility, but due to lack of focus, you miss many of them.
When a claim application is denied or even any oversight occurs during the process, you don’t miss a revenue opportunity you weaken your facility’s wealth.
Here are other things to strictly avoid in your RCM strategy:
| Practice to Avoid | Description | Consequence |
| Inaccurate Patient Data | Errors in patient information such as name, DOB, or insurance details | Leads to claim denials and delays in payment |
| Lack of Staff Training | Insufficient training on coding, billing, and compliance | Increases errors, compliance risks, and inefficiencies |
| Delayed Claim Submission | Procrastination in submitting claims to payers | Results in missed deadlines, denials, and cash flow issues |
| Poor Documentation | Incomplete or inaccurate medical documentation | Causes claim denials, legal issues, and revenue loss |
| Ignoring Denial Management | Failing to track and analyze denied claims | Leads to repeat denials and lost revenue |
| Non-compliance with Regulations | Ignoring or being unaware of healthcare regulations | Results in legal penalties, fines, and reputational damage |
| Manual Billing Processes | Relying on manual entry for billing | Increases the risk of errors and inefficiencies |
| Inadequate Follow-up on A/R | Not following up on outstanding accounts receivable | Results in uncollected revenue and higher write-offs |
| Lack of Communication with Patients | Failing to communicate billing details and payment options | Leads to patient dissatisfaction and payment delays |
| Overlooking EHR and Technology Updates | Not keeping systems and software up to date | Causes security vulnerabilities, inefficiencies, and non-compliance |
For small health practices, it becomes even 100X more important to conduct RCM revenue cycle management properly.
Since they have less amount of claims and patient bills, any of them shouldn’t be missed in order to keep running the health facility.
All this shows that paying focus to RCM revenue cycle management can directly and positively affect your revenue generation capacity. All of this is only possible when you are attentive enough to conduct each RCM step with full proficiency.
RCM Revenue Cycle Management Quality Checks
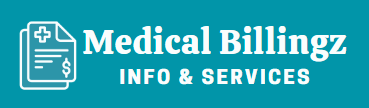
To help you level up your RCM revenue cycle management in your health facility, here are 7 quality checks you must make sure. That will aid you in strengthening your hospital’s financial stability.
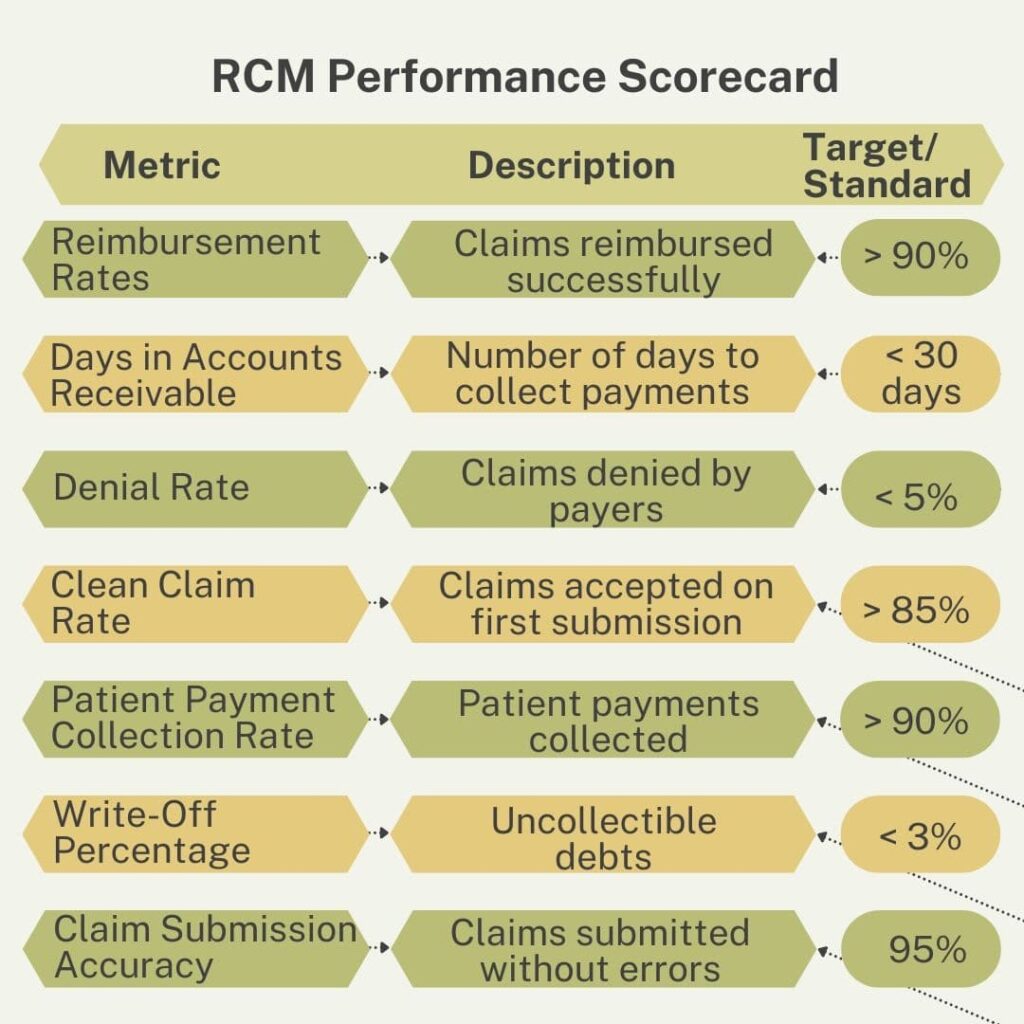
1. Verify Insurance Eligibility
When patients get treatment, if they have health insurance, their charges will be covered according to their insurance package. Still, there is some amount called deductibles and co-payments that they have to pay.
But sometimes lack of patient’s insurance details results in misleading filling of claim forms, that in return confront claim denial.
In order to avoid claim rejection in RCM revenue cycle management, you must do extra efforts in verifying patients’ insurance coverage, how much their insurance will cover, and how much they have to pay.
Verify the following things:
- Patient demographic data
- Benefit list according to the patient’s plan
- Compare the total bill amount with deductibles, copayments, and insurance
- Primary and secondary insurance coverage
- Code benefits
- The max coverage limit for a specific treatment
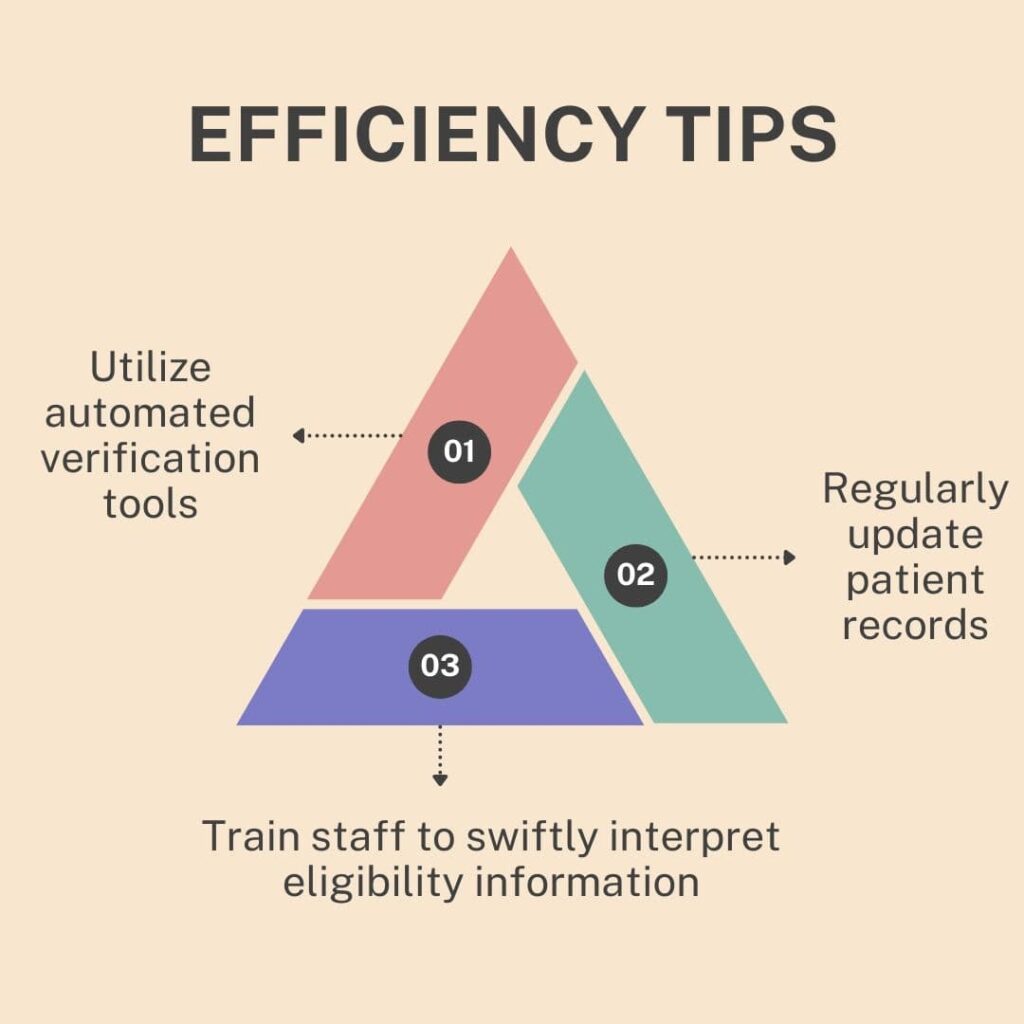
2. Code Audits
The decision of whether reimbursement will be made or not highly depends on medical coding during RCM revenue cycle management. Any mistake in the code may lead to problem identification by the payer and quick rejection of the claim.
Most of the time, coding staff while dealing with hundreds of claims a day, make manual as well as systematic errors in claim applications.
You must make sure to train them to provide quality-level health services, so you don’t miss a revenue opportunity.
Additionally, you must also conduct regular medical coding audits. It will help you study data and trends for claim approval and rejection, on the basis of which you can make informed decisions.
3. Study A/R
AR is the process of keeping a regular follow-up with the claim. Your health facility must keep up with the claim applications to track their status.
This is specifically helpful after claim denial and during application delay.
Don’t make the mistake to leave your claim unfollowed, because the more time taken by a claim application, the more it weakens the chances of getting a reimbursement.
Make sure your claims are paid within 30 days.
Keep the records and updated status info of claim applications, quickly resolve any objection by the insurance payer and immediately re-submit the application to get the payment.
4. Difference Between Charged And Paid Claims
From countless claim applications during RCM revenue cycle management, where some reject and some are paid, many claims are also underpaid, either due to lack of charges recognition by the payer or any other reason.
When you are paid less than what you charge, it can have negative impacts on your ability to provide top-standard healthcare facilities.
Keep up with the claim applications, and make sure each is paid. If there is any underpaid claim, communicate with the payer and execute constant appeals to ensure full payment.
5. Write-Off Percentage
A write-off is a process in which you are paid less than the actual amount. Analyze the rate of write-offs and act accordingly.
You must perform some potential procedures to write-offs and get your claim, which will further enhance your revenue generation during RCM revenue cycle management.
6. Ratio Of Paid And Denied Claims
Irrespective of your utmost struggle to get the claims approved, some of the claims keep going rejected, and you can’t stop them.
The only solution is to study the ratio between paid and denied claims to know your lacking areas, which will help you reduce claim denials.
Study claims denial and accepting data on a weekly or monthly basis. Observe what mistakes lead to claim denials and what were applications that got accepted immediately.
Based on the facts, take cautious future RCM revenue cycle management steps and maximize your potential to collect reimbursement.
7. Physician Credentialing
Making sure your physicians are eligible enough to provide health services and comply with health regulations will help you get greater reimbursement.
This is due to the fact that insurance payers prefer only those health facilities and their claim applications that have verified physicians. They are more likely to pay when the health services are provided by qualified physicians.
For this, conduct timely physician credentialing. You must also keep an eye on re-credentialing dates, and make sure all your physicians are eligible to provide health services.
Conclusion
RCM revenue cycle management is not a complicated process at all, yet many health facilities fail to conduct it accurately. No matter on what scale you provide health services, always follow these quality checks to get your deserved revenue.
Besides use these technologies in RCM to maximize your efforts:
| Technology | Functionality | Benefits |
| Electronic Health Records (EHR) | Centralized patient information storage and management | Reduces data entry errors, improves data accessibility, and streamlines patient care coordination |
| Automated Billing Systems | Automates the billing and claims submission process | Increases efficiency, reduces manual errors, accelerates revenue cycle, and ensures timely reimbursements |
| Predictive Analytics | Analyzes historical data to forecast financial outcomes and identify trends | Helps in identifying potential issues early, optimizes revenue cycle management, and improves decision-making |
| Patient Portals | Provides patients access to their health information, billing, and payment options | Enhances transparency, improves patient engagement, reduces administrative workload, and increases payment collections |
| Revenue Cycle Management Software | Integrates various RCM processes such as billing, coding, and claims management | Streamlines workflows, improves accuracy, enhances compliance, and provides real-time financial reporting |
| Telehealth Platforms | Facilitates remote patient consultations and care delivery | Expands patient access, improves patient satisfaction, and generates additional revenue streams |
| Artificial Intelligence (AI) | Uses machine learning algorithms to automate and optimize RCM tasks | Improves accuracy in coding and billing, detects fraud, reduces denials, and enhances overall efficiency |
| Robotic Process Automation (RPA) | Automates repetitive and rule-based tasks within the RCM process | Reduces human error, increases processing speed, and frees up staff for more complex tasks |
But if you can’t conduct RCM revenue cycle management by yourself, opt for outsourcing RCM. As many revenue management companies are awaiting to implement their claim management experience to help you secure adequate reimbursement.