What is medical associate billing?
Medical associates billing refers to the structured process of preparing, submitting, and following up on claims with health insurance companies to receive payment for services provided by healthcare professionals. It ensures that physicians, clinics, and hospitals get reimbursed accurately and on time.
Importance in modern healthcare practices
As healthcare becomes increasingly complex, medical associate plays a critical role in maintaining financial stability. Efficient billing processes not only maximize reimbursements but also reduce administrative burdens, allowing healthcare providers to focus more on patient care.
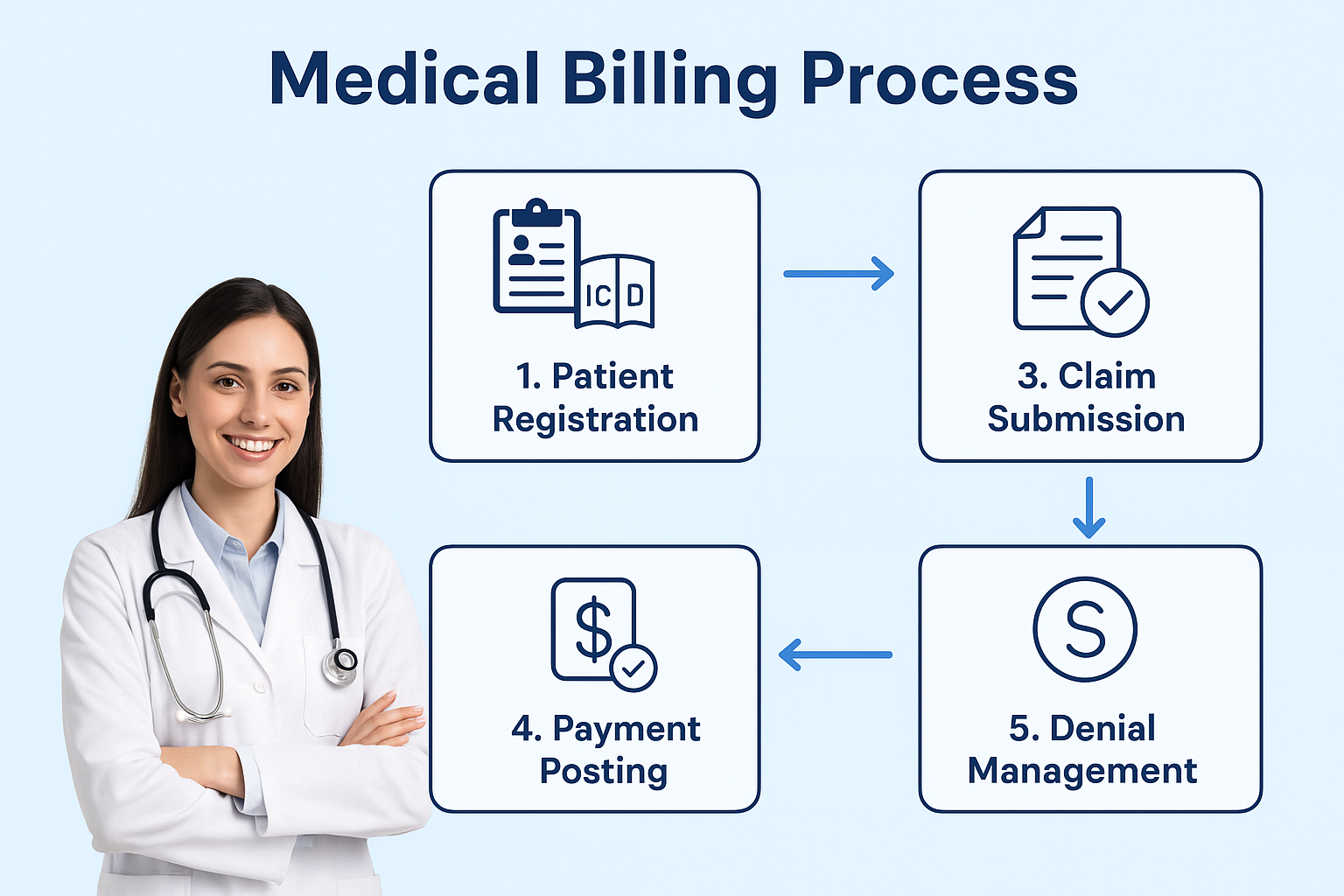
Overview of the revenue cycle process
The revenue cycle begins with patient registration and ends with the successful collection of payments. This cycle involves multiple steps such as coding, claim submission, payment posting, and denial management. Proper handling of this process ensures steady cash flow for healthcare organizations.
2. Understanding the Basics of Medical Associate
Definition and scope of billing services
Medical associate billing includes a wide range of tasks, from collecting patient demographics to handling denied claims. It requires attention to detail, compliance with industry standards, and effective communication with insurance providers.
Role of Medical Billing Associates in Modern Healthcare Practices
Difference between billing and coding
While coding involves translating medical services into standardized codes (ICD, CPT, HCPCS), billing focuses on preparing claims using these codes to ensure accurate reimbursement. Both functions work hand in hand to streamline healthcare payments.
Role of medical billing associates in healthcare
Medical Billing associates act as a bridge between providers, patients, and insurance companies. They ensure that all claims are processed correctly, reducing financial losses and improving revenue cycles.
3. Why Medical Associates is Essential
Ensuring accurate reimbursements
Accurate billing guarantees that healthcare providers receive fair payment for the services they deliver, preventing revenue leakage.
Reducing claim denials and rejections
By verifying insurance eligibility and using correct codes, billing associates minimize denials and speed up the reimbursement process.
Enhancing patient satisfaction through transparent billing
Patients appreciate clear and accurate billing statements, which build trust and improve the overall care experience.
4. Key Components
4.1 Patient Information Management
- Registration and demographic data collection: Correct patient data is essential to avoid claim rejections.
- Insurance verification and eligibility checks: Ensures services are covered and reduces financial risks.
4.2 Medical Coding and Documentation
- Importance of ICD, CPT, and HCPCS codes: Standardized codes form the foundation of billing.
- Common coding errors to avoid: Inaccurate codes can result in claim denials and compliance issues.
4.3 Claim Submission
- Paper vs. electronic claims (EDI): Electronic submissions reduce delays and improve accuracy.
- Timely filing guidelines: Each payer hasuthat must be met to avoid non-payment.
4.4 Payment Posting and Reconciliation
- Recording payments from insurance and patients: Ensures correct allocation of payments.
- Identifying underpayments and discrepancies: Helps maintain accurate financial records.
4.5 Denial Management
- Common reasons for claim denials: Missing information, coding errors, and eligibility issues.
- Strategies to appeal and resolve rejected claims: Proactive follow-ups improve revenue recovery.
Explore in-depth guides and tutorials to master medical billing systems and processes.
5. Challenges
- Frequent coding and documentation errors: Even minor mistakes can result in claim rejection.
- Compliance with HIPAA and federal regulations: Strict rules must be followed to protect patient data.
- Dealing with changing payer policies: Constant updates in insurance requirements create challenges.
- Administrative and staffing challenges: High workloads can lead to burnout among billing teams.
6. Best Practices for Effective Medical Associates
- Staff training and certifications: Continuous education ensures billing associates stay updated.
- Conducting regular audits and error checks: Prevents revenue leakage and ensures compliance.
- Improving communication between providers and patients: Builds trust and reduces disputes.
- Tracking Key Performance Indicators (KPIs) for billing efficiency: Helps measure success and identify areas of improvement.
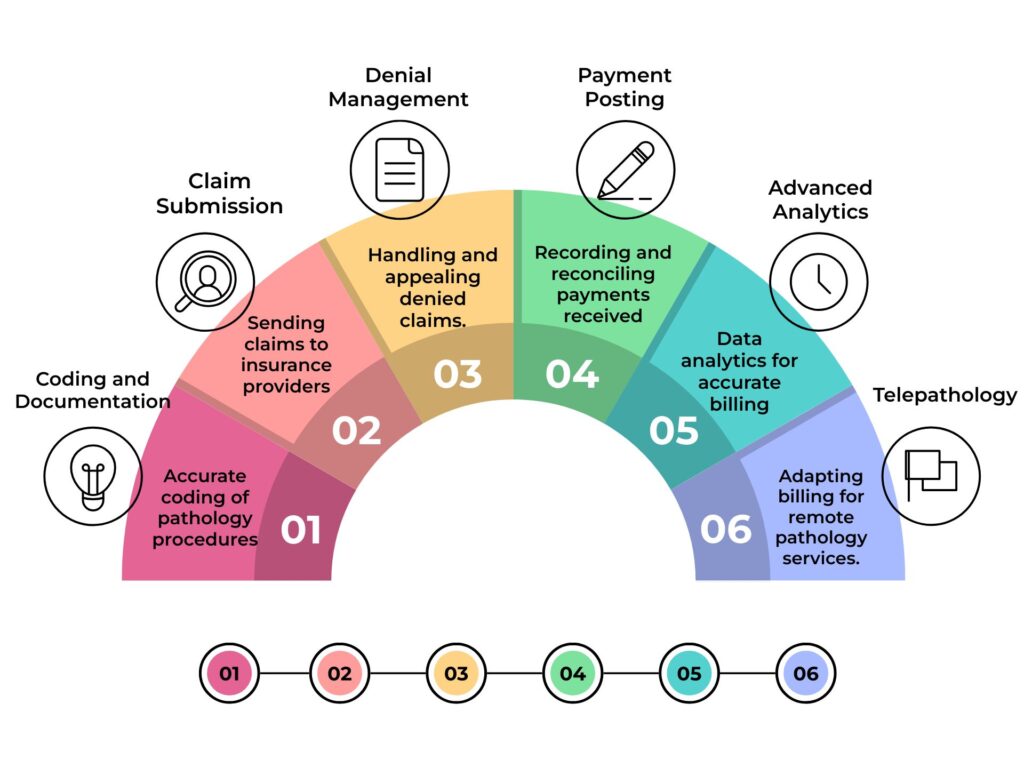
7. Technology and Automation in Medical
- Benefits of electronic health records (EHR) integration: Streamlines documentation and billing.
- Role of AI and machine learning in billing automation: Reduces manual errors and improves efficiency.
- Cloud-based billing software for efficiency: Provides accessibility and reduces infrastructure costs.
- Data security and compliance with digital tools: Protects sensitive patient and financial data.
8. Outsourcing
- Advantages of outsourcing to billing companies: Reduces workload and increases efficiency.
- Cost efficiency vs. in-house billing: Outsourcing is often more affordable for smaller practices.
- How to choose the right medical billing partner: Evaluate experience, compliance, and support services.
- Key questions to ask before outsourcing: Understand pricing models, data security measures, and reporting practices.
| Aspect | Short Description |
|---|---|
| Patient Registration | Collecting accurate details |
| Insurance Verification | Checking eligibility & plans |
| Medical Coding | Using ICD, CPT, HCPCS codes |
| Claim Submission | Paper or EDI-based process |
| Payment Posting | Recording and reconciling |
| Denial Management | Handling rejected claims |
9. Future of Medical Associate Billing
- Trends in telehealth billing and virtual care: New billing models are emerging with telemedicine.
- Blockchain technology for secure transactions: Provides transparency and minimizes fraud.
- Value-based care and its impact on billing models: Payment models are shifting toward patient outcomes.
- Predictions for the next decade in healthcare billing: Expect more automation, stronger compliance, and global integration.
10. Conclusion
Recap of the role of medical billing in healthcare
Medical associate billing is the backbone of revenue cycle management, ensuring accurate reimbursements and regulatory compliance.
Benefits for providers, insurers, and patients
With streamlined processes, providers gain financial stability, insurers process claims faster, and patients receive clear, transparent billing.
Final thoughts on optimizing billing practices
As technology advances and healthcare evolves, partnering with trained Medical Billing associates and adopting best practices will remain vital for success.
FAQs
Can small healthcare practices benefit from outsourcing billing?
Yes. Outsourcing can help small practices reduce administrative burdens, save costs, and improve efficiency by leveraging the expertise of specialized billing companies.
What are the common challenges in medical billing?
Some challenges include frequent coding errors, changing insurance policies, HIPAA compliance requirements, and high denial rates. Proper training, audits, and automation can help overcome these issues.
How does technology improve the billing process?
Electronic Health Records (EHR), AI-driven billing tools, and cloud-based software reduce errors, speed up claim submission, and ensure better compliance with payer guidelines.
What role do Medical Billing associates play in denial management?
They identify the reasons behind denied claims, make necessary corrections, and resubmit appeals. Effective denial management improves cash flow and reduces revenue loss.
Is medical billing affected by telehealth services?
Yes. Telehealth introduces new billing codes and reimbursement models. Billing associates must stay updated with payer policies to ensure accurate claim processing for virtual care.