In the healthcare industry, claim rate improvement is a crucial factor in ensuring timely and accurate reimbursements from insurance companies. With growing complexities in coding, compliance, and payer requirements, providers must adopt effective strategies to enhance their claim acceptance rates.
Understanding Claim Rate in Medical Billing
The claim rate refers to the percentage of medical claims that are accepted and reimbursed by insurance payers without rejections or denials. A high claim rate means that most claims submitted are approved on the first submission, leading to faster cash flow and fewer administrative burdens.
Claim rate improvement involves reducing claim denials, minimizing resubmissions, and increasing the percentage of clean claims. Clean claims are those that pass through the system without needing corrections, which accelerates the reimbursement cycle and reduces overhead costs.

Why Claim Rate Improvement Matters
Medical practices rely heavily on reimbursements from third-party payers to maintain cash flow. A poor claim rate can result in delayed payments, increased administrative work, and loss of revenue. Focusing on claim rate improvement ensures that billing processes are streamlined and error-free.
High-performing medical billing systems can achieve claim acceptance rates of 95% or higher. This level of efficiency not only reduces operational costs but also improves the financial stability of healthcare providers. In contrast, low claim rates signal a need for urgent improvements in workflow, coding accuracy, and payer compliance.
Common Causes of Low Claim Rates
Improving claim rates starts with identifying the root causes of denials and rejections. Some of the most frequent reasons include:
- Incorrect or missing patient information
- Improper coding or outdated ICD/CPT codes
- Failure to verify insurance eligibility
- Duplicate claims
- Lack of required documentation
- Non-compliance with payer-specific guidelines
Understanding these challenges is essential to implementing effective strategies for claim rate improvement.
Unlock faster payments and fewer billing errors.
Key Strategies for Claim Rate Improvement
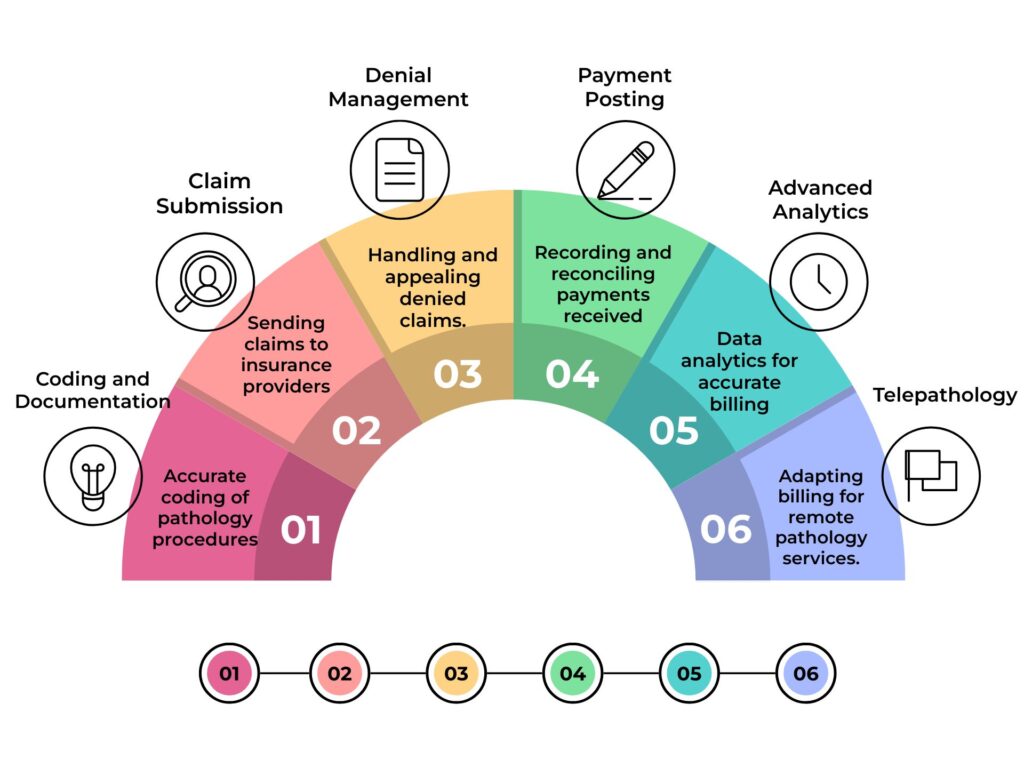
1. Accurate and Complete Documentation
Detailed clinical documentation is the foundation of clean claims. Providers must ensure that each encounter is properly recorded with supporting medical necessity and accurate diagnosis and procedure codes. Consistent training and quality assurance processes can help reduce documentation-related errors.
2. Real-Time Insurance Verification
Verifying patient insurance coverage before services are rendered prevents issues related to eligibility denials. Use real-time verification tools to confirm active coverage, copays, deductibles, and plan limitations. This proactive step is vital for effective claim rate improvement.
3. Automated Claim Scrubbing
Claim scrubbing software checks claims for errors before submission. These tools catch common issues such as incorrect modifiers, missing data, and coding mismatches. Integrating automated scrubbing systems into the billing workflow significantly increases the clean claim rate and enhances claim rate improvement.
4. Staff Training and Coding Accuracy
Medical coders and billing staff must stay current with the latest coding updates, payer policies, and compliance rules. Regular training and certification programs ensure that teams are knowledgeable and equipped to prevent coding errors that lead to denials.
5. Regular Claims Auditing
Conducting internal audits helps identify patterns in denied or rejected claims. By analyzing these patterns, billing teams can address systemic issues, refine their processes, and reinforce protocols that support claim rate improvement.
The Role of Technology in Claim Rate Improvement
Technology plays a transformative role in streamlining medical billing and optimizing the claim process. From AI-driven claim analytics to integrated revenue cycle management (RCM) platforms, healthcare organizations can leverage automation to reduce manual errors and accelerate claim turnaround.
Electronic Health Records (EHR) systems integrated with assignment of benefits in aob billing software provide a seamless flow of information from clinical documentation to billing. This reduces the risk of data entry errors and supports real-time error checks before claim submission.
Additionally, machine learning algorithms can predict claim denial trends and suggest preventive actions, aiding in ongoing claim rate improvement efforts.
Measuring the Success of Claim Rate Improvement
To determine the effectiveness of initiatives, healthcare providers should track key performance indicators (KPIs) such as:
- First-pass claim acceptance rate
- Average days in A/R (accounts receivable)
- Claim denial rate
- Percentage of clean claims
- Time to payment
Improvements in these KPIs reflect a successful claim rate improvement strategy and indicate that the organization is optimizing its revenue cycle effectively.
Table: Factors and Solutions for Claim Rate Improvement
| Common Issue | Effective Solution |
|---|---|
| Incomplete patient information | Use automated intake verification |
| Coding inaccuracies | Regular coder training sessions |
| Eligibility errors | Implement real-time eligibility checks |
| Claim formatting issues | Employ claim scrubbing software |
| Outdated payer guidelines | Regular payer policy updates |
| High denial volume | Conduct monthly denial audits |
Maintaining Long-Term Claim Rate Improvement
Claim rate improvement is not a one-time project but a continuous effort. To sustain high claim rates, providers must build a culture of accountability and ongoing education. Establishing a feedback loop between coders, clinicians, and billing staff ensures that errors are identified and corrected promptly.
Additionally, staying updated with evolving payer rules and industry regulations such as HIPAA, ICD-11 transitions, and CMS guidelines is critical to maintaining billing accuracy and compliance.
Engaging with external billing consultants or outsourcing to specialized RCM vendors can also enhance the billing process and drive claim rate improvement, especially for small to mid-sized practices lacking in-house expertise.
Is Your Medical Practice Losing Money? Discover the Right RCM Tools
Financial Benefits of Claim Rate Improvement
Improving claim rates not only reduces denials but also leads to faster reimbursements and improved cash flow. This increased efficiency lowers the cost per claim and frees up staff to focus on patient care rather than administrative burdens.
Moreover, as the healthcare reimbursement landscape becomes increasingly value-based, accurate and timely billing becomes essential to maximize revenue and avoid penalties. Claim rate improvement helps healthcare organizations thrive financially while maintaining compliance with industry standards.
Conclusion: A Strategic Imperative for Healthcare Providers
In today’s competitive healthcare environment, claim rate improvement is not optional—it is a strategic necessity. By adopting proactive measures such as accurate documentation, automation tools, staff training, and regular audits, healthcare providers can significantly enhance their billing efficiency and financial performance.
Through a focus on continuous improvement and technological innovation, practices can reduce the risk of denials, accelerate payments, and build a more resilient revenue cycle. Ultimately, claim rate improvement leads to better financial outcomes and allows providers to focus more on delivering quality care.
FAQs
How can I improve my medical billing claim rate?
You can improve your claim rate by:
- Ensuring accurate documentation and coding
- Verifying insurance eligibility in real time
- Using claim scrubbing software
- Training staff regularly
- Performing internal audits
- Leveraging technology like EHR and AI tools
What is a “clean claim” and how does it relate to claim rate improvement?
A clean claim is a medical claim submitted without errors or omissions that gets accepted by the payer without needing corrections. Maximizing clean claims is the cornerstone of effective claim rate improvement.
Can software really help with claim rate improvement?
Yes, modern billing software with automated claim scrubbing, real-time eligibility checks, and denial management features plays a crucial role in achieving consistent claim rate improvement. It reduces human error and speeds up the reimbursement process.
How often should I audit my medical claims for better results?
Regular monthly or quarterly audits are recommended. They help identify recurring errors, track performance metrics, and implement targeted improvements to sustain ongoing claim rate improvement.