Behavioral Health Revenue Cycle Management (RCM) is a core component of any healthcare organization’s financial health. In behavioral health practices, where services range from counseling sessions to psychiatric evaluations, ensuring accurate and timely payment can be more challenging than in other medical specialties. This is because behavioral health billing often involves complex codes, varying session lengths, and frequent coordination with insurance providers. Understanding how to optimize the process can greatly improve operational efficiency and cash flow.
Importance of Streamlined Processes
Streamlining the medical billing process in behavioral health revenue cycle management care is crucial. A smooth workflow not only reduces administrative burden but also ensures that practitioners can focus more on patient care. This includes having clear protocols for patient intake, verifying insurance coverage upfront, and following precise coding guidelines. A well-organized revenue cycle also reduces claim rejections, ultimately improving the financial stability of the practice.
Core Steps in Behavioral Health Revenue Cycle Management
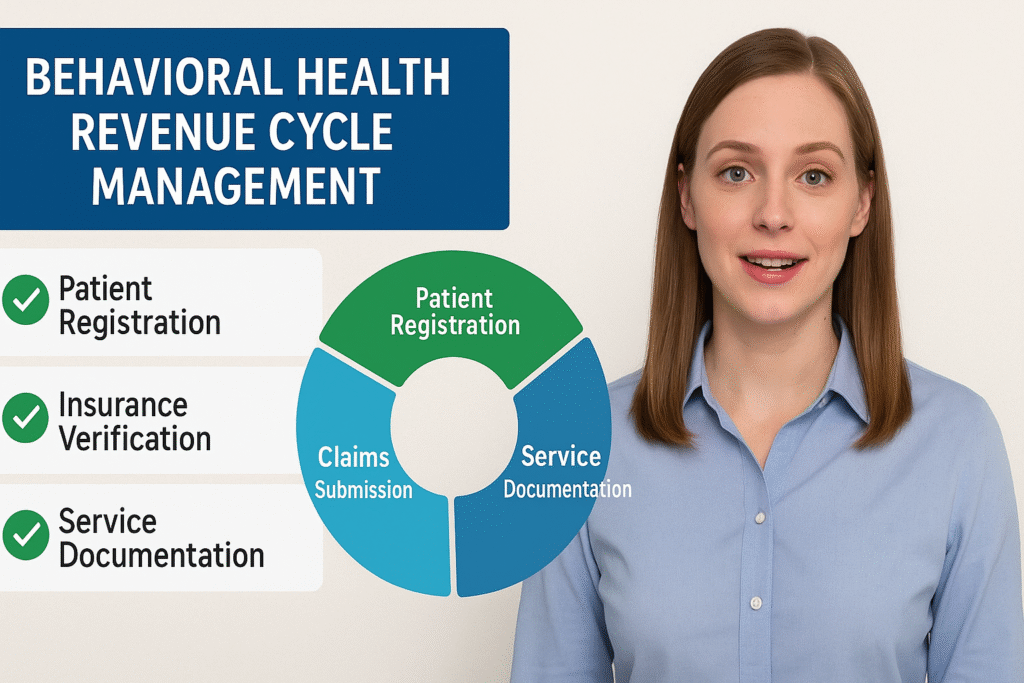
While the fundamentals of RCM apply across healthcare sectors, the behavioral health field requires certain tailored steps for optimal results. The main stages include:
- Patient Registration and Insurance Verification – Collecting complete demographic and insurance information upfront to avoid claim errors.
- Service Documentation – Detailed and accurate clinical notes that meet payer requirements.
- Coding and Charge Entry – Applying the correct CPT and ICD-10 codes based on the service provided.
- Claims Submission – Timely electronic submission to reduce delays.
- Payment Posting – Recording payments accurately and reconciling with claims.
- Denial Management – Identifying patterns in denied claims and implementing corrective actions.

Regulatory Compliance in Behavioral Health Billing
Compliance is a non-negotiable part of the RCM process. Behavioral health providers must adhere to HIPAA regulations to safeguard patient data, as well as follow payer-specific guidelines. Additionally, compliance with medical necessity requirements is critical especially for mental health services, where insurers may require proof of ongoing treatment need. Failure to meet these standards can result in claim denials and even legal penalties.
The Role of Technology in Optimizing RCM
Modern billing software and electronic health record (EHR) systems have revolutionized revenue cycle management. For behavioral health practices, integrated solutions can automate tasks such as eligibility checks, coding assistance, and claim tracking. Artificial intelligence tools are also being adopted to predict denial risks and suggest corrections before submission. Technology reduces human error, improves transparency, and speeds up payment cycles.
Impact of Staff Training on Revenue Cycle Efficiency
Even the best systems require knowledgeable staff to operate them effectively. Training billing teams in behavioral health-specific coding rules, payer requirements, and denial prevention strategies ensures smoother claim processing. Ongoing education also keeps staff updated with regulatory changes, such as CPT code revisions or new payer policies.
Common Causes of Claim Denials in Behavioral Health
In behavioral health billing, claim denials often occur due to incomplete documentation, incorrect coding, expired authorizations, and mismatches between the billed service and the patient’s coverage. Identifying and addressing these root causes is essential for improving the revenue cycle. Preventive measures, such as pre-authorization verification and double-checking documentation, can drastically reduce denial rates.
Looking to improve your practice’s billing efficiency? Understanding key billing principles
Financial Benefits of a Strong RCM Process
A robust RCM system directly influences a practice’s profitability. Faster claims processing leads to quicker reimbursements, improved cash flow, and reduced accounts receivable days. By minimizing rework on denied claims, staff can allocate more time to other productive tasks. In addition, efficient processes enhance patient satisfaction by reducing billing disputes and providing transparent cost information.
Table: Key Elements of Behavioral Health Billing Optimization
| Process Step | Best Practice |
|---|---|
| Insurance Verification | Confirm coverage before service |
| Accurate Coding | Use correct CPT/ICD-10 codes |
| Timely Claims Submission | Submit electronically |
| Detailed Documentation | Meet payer requirements |
| Denial Tracking | Identify recurring issues |
| Staff Training | Ongoing education programs |
Future Trends in Behavioral Health Revenue Cycle Management
The future of behavioral health billing will be shaped by evolving technology and value-based care models. Automation will further reduce manual work, while data analytics will enable providers to identify patterns and optimize their revenue cycles proactively. Telehealth, which has expanded significantly, will require specialized billing approaches to ensure correct reimbursement.
How Outsourcing Can Improve Efficiency
Many behavioral health practices are now outsourcing their RCM to specialized billing companies. Outsourcing can bring expertise, advanced technology, and scalable processes that may be difficult to maintain in-house. It allows providers to focus entirely on patient care while experts handle claim submissions, follow-ups, and payment posting. This strategy is especially useful for smaller practices with limited administrative staff.
Challenges
Complex Coding Requirements – Behavioral health services often require multiple CPT and ICD-10 codes, and errors can lead to denials.
Frequent Authorization Needs – Many insurers demand prior approvals, causing delays if not managed promptly.
High Claim Denial Rates – Denials often result from incomplete documentation or mismatched codes.
Inconsistent Session Structures – Varying appointment lengths and service types complicate billing accuracy.
Regulatory Compliance Pressure – Strict privacy and documentation laws require constant staff vigilance to avoid violations.
Key Steps to a Complete RCM Process in Behavioral Health
The behavioral health RCM process begins with accurate patient intake, insurance verification, and service documentation. Each step, from coding to claims submission, plays a crucial role in ensuring timely reimbursements.
Front-End vs. Back-End in Behavioral Health Medical Billing
The front-end covers tasks before and during patient care, such as eligibility checks and coding accuracy. The back-end focuses on payment posting, denial management, and follow-up to secure revenue.
Improving Behavioral Health Revenue Cycle Management: Best Practices
Implementing pre-authorization checks, regular staff training, and denial tracking can optimize the RCM process. These practices reduce claim errors and boost financial performance.
Step-by-Step RCM Workflow for Behavioral Health Practices
A structured workflow starts with patient registration, followed by documentation, coding, claims submission, payment posting, and denial resolution. Consistency in each stage ensures fewer rejections and faster payments.
Looking for tips to speed up the payment process in healthcare billing?
Strategies to Strengthen Behavioral Health Revenue Cycle Management
Automation, data analytics, and outsourcing can help address bottlenecks in the RCM process. Regular audits and process reviews further improve efficiency and compliance.
Compliance, Privacy & Regulatory Considerations in Behavioral Health RCM
Providers must adhere to HIPAA regulations and payer-specific rules to avoid legal or financial penalties. Strong data security measures and accurate documentation are essential for compliance.
Conclusion
Efficient behavioral health revenue cycle management is vital for maintaining the financial health of a practice. By addressing the unique challenges of behavioral health billing—such as complex coding, strict documentation, and frequent authorizations—providers can significantly reduce payment delays and claim denials. Leveraging technology, training staff, and even outsourcing can enhance operational efficiency, ensuring that practitioners can focus on delivering high-quality care without financial disruptions.
FAQs
What are the biggest challenges in behavioral health billing?
Common challenges include complex coding, prior authorization requirements, incomplete documentation, high denial rates, and strict compliance regulations.
How can technology improve behavioral health RCM?
Billing software and EHR integration automate coding, track claims in real time, and flag errors before submission, reducing delays and denials.
What are some best practices for behavioral health revenue cycle management?
Best practices include verifying insurance before services, maintaining detailed documentation, training billing staff, and regularly auditing the process.
Should behavioral health practices outsource their RCM?
Outsourcing can save time and improve accuracy, especially for smaller practices, by leveraging expert knowledge and advanced billing technology.

