Accounts Receivable Management in medical billing plays a crucial role in maintaining the financial health of healthcare providers. It involves tracking and collecting payments for medical services rendered to patients, ensuring a steady cash flow for medical practices, hospitals, and clinics. Effective Accounts Receivable Management (ARM) helps in minimizing revenue loss, reducing outstanding claims, and improving overall financial performance.
Understanding Accounts Receivable in Medical Billing
Accounts receivable (AR) in medical billing refers to the outstanding balance that patients or insurance companies owe to healthcare providers for services rendered. These unpaid claims and invoices are a significant part of a healthcare facility’s revenue cycle. The efficiency of Accounts Receivable Management determines the provider’s ability to maintain financial stability while ensuring timely reimbursement.
The Revenue Cycle Process in Medical Billing
- Patient Registration: Collecting patient demographic and insurance details.
- Insurance Verification: Confirming insurance coverage and eligibility.
- Medical Coding and Billing: Converting diagnoses and procedures into standardized codes for claim submission.
- Claim Submission: Sending claims to insurance companies for reimbursement.
- Claim Processing and Payment Posting: Receiving payments and updating records.
- Accounts Receivable Follow-up: Tracking unpaid claims and pursuing collections.
- Denial Management and Appeals: Handling denied claims and resubmitting them.
Importance of Accounts Receivable Management in Medical Billing
Effective Accounts Receivable Management is critical for ensuring that healthcare providers receive timely payments and maintain a positive cash flow. Key benefits include:

1. Enhanced Cash Flow
By streamlining Accounts Receivable Management, medical practices can reduce the time it takes to receive payments from insurance companies and patients. Faster collections lead to improved cash flow, which is essential for operational stability.
2. Reduction in Outstanding Claims
Unresolved claims can lead to revenue loss. Implementing a robust Accounts Receivable Management strategy helps in reducing the number of outstanding claims by ensuring timely follow-ups and claim resubmissions.
3. Minimized Denials and Rejections
Claims are often denied due to errors in coding, incorrect patient information, or insurance discrepancies. A strong Accounts Receivable Management system identifies these issues early, reducing denials and ensuring faster reimbursements.
4. Improved Patient Satisfaction
Clear billing practices and transparent communication regarding patient financial responsibilities help in building trust. Efficient Accounts Receivable Management reduces confusion over payments, leading to a better patient experience.
5. Regulatory Compliance
Healthcare providers must comply with regulations such as HIPAA and CMS guidelines. Proper Accounts Receivable Management ensures compliance with billing and coding standards, reducing the risk of audits and penalties.
How to Improve Accounts Receivable Management in Healthcare?
Challenges in Accounts Receivable Management
Despite its importance, Accounts Receivable Management in medical billing comes with various challenges:
1. Delayed Payments from Insurance Companies
Insurance companies may take longer than expected to process claims, leading to payment delays. This affects the provider’s ability to maintain cash flow.
2. High Claim Denial Rates
Errors in coding, missing information, and policy limitations result in claim denials. Without an efficient denial management system, these claims remain unpaid.
3. Patient Payment Delays
Patients often struggle to understand medical bills, leading to delayed payments. The lack of convenient payment options can further complicate collections.
4. Complex Billing and Coding Regulations
Healthcare billing involves stringent regulations that change frequently. Keeping up with these changes is necessary to avoid claim denials and revenue loss.
5. Inefficient Follow-up Processes
If healthcare providers do not follow up on outstanding payments efficiently, accounts receivable balances continue to grow, leading to financial instability.
Best Practices for Optimizing Accounts Receivable Management
To improve Accounts Receivable Management, healthcare providers can implement the following best practices:
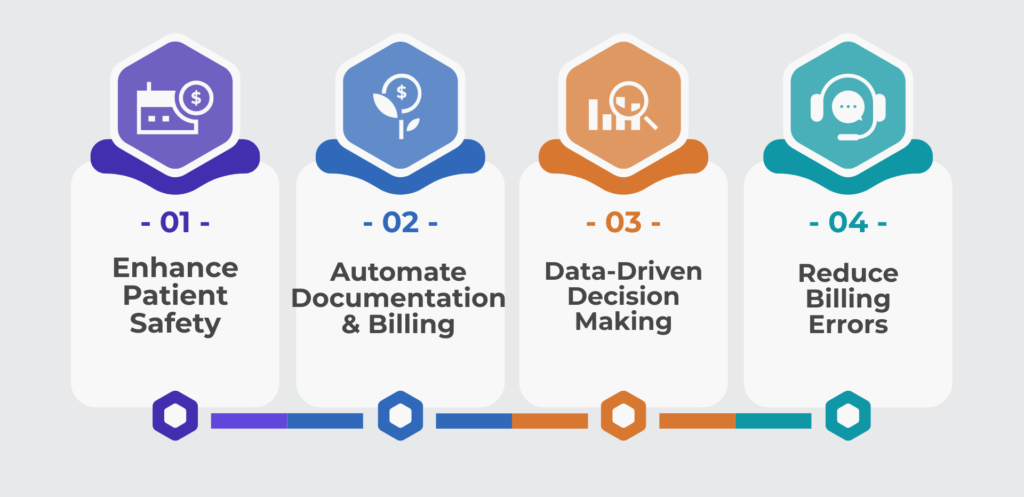
1. Implement Automated Billing Systems
Automation helps streamline the billing process, reducing errors and ensuring timely claim submissions. Electronic Health Records (EHR) and practice management software can enhance efficiency.
2. Verify Insurance Information Before Treatment
Verifying patient insurance coverage before providing treatment helps prevent claim denials due to eligibility issues.
3. Submit Clean Claims
Ensuring that claims are error-free before submission increases the likelihood of approval. Double-checking codes, patient details, and insurance information is essential.
4. Establish a Robust Follow-up System
A dedicated team should track outstanding claims and follow up with insurance companies and patients regularly. Setting up reminders and automated notifications can help.
5. Offer Multiple Payment Options for Patients
Providing online payment portals, credit card payments, and installment plans can encourage patients to pay their dues on time.
6. Analyze AR Reports Regularly
Generating detailed accounts receivable reports helps identify trends, track overdue payments, and make informed financial decisions.
7. Train Staff on Billing and Coding Regulations
Regular training sessions ensure that staff members stay updated on the latest medical billing regulations, minimizing claim denials.
Strategies to Reduce Accounts Receivable Aging
Aging accounts receivable refers to unpaid invoices that have been outstanding for an extended period. To minimize AR aging, providers can:
1. Categorize AR Based on Aging Periods
Grouping AR into 30, 60, 90, and 120+ day categories helps prioritize collections based on the highest-risk accounts.
How Can Medical Practices Reduce Outstanding Accounts Receivable?
2. Contact Patients Early
Sending reminders to patients before their payment due date can reduce late payments.
3. Follow Up on Denied Claims Immediately
Appealing denied claims as soon as possible improves the chances of receiving payment.
4. Use Collection Agencies for Unpaid Accounts
For significantly overdue accounts, partnering with a collection agency can help recover payments.
Table: Key Aspects of Accounts Receivable Management
| Aspect | Description |
|---|---|
| Cash Flow Management | Ensuring steady revenue through timely collections |
| Claim Denial Reduction | Minimizing errors to prevent claim rejections |
| Automated Billing Systems | Using technology to streamline billing |
| Patient Payment Plans | Offering flexible payment options for patients |
| AR Follow-Up Strategies | Regular tracking and reminders for unpaid claims |
| Compliance with Regulations | Adhering to billing laws and coding standards |
Conclusion
Effective Accounts Receivable Management in medical billing is essential for the financial success of healthcare providers. By implementing best practices such as automation, timely follow-ups, and improved patient communication, medical practices can optimize their revenue cycle and reduce outstanding payments. Addressing challenges such as claim denials, delayed reimbursements, and regulatory compliance ensures smooth operations and financial stability. As healthcare billing continues to evolve, adopting proactive Accounts Receivable Management strategies will help providers maintain efficiency and profitability.
FAQs
How can healthcare providers reduce claim denials?
Providers can reduce claim denials by verifying insurance details before treatment, submitting accurate claims, training staff on coding regulations, and promptly addressing denied claims.
What role does automation play in Accounts Receivable Management?
Automation streamlines medical billing, reduces errors, speeds up claim submissions, and improves tracking of unpaid invoices, leading to faster collections and reduced AR aging.
How can patients be encouraged to pay their medical bills on time?
Offering multiple payment options, clear billing communication, automated reminders, and flexible installment plans can encourage patients to pay their medical bills promptly.
How often should AR reports be reviewed?
AR reports should be reviewed regularly, at least monthly, to identify outstanding claims, assess payment trends, and take necessary actions to optimize collections.