Healthcare providers must submit their claims quickly and effectively in order to be reimbursed on time. In order to facilitate communication between healthcare providers, a clearinghouse claims submission is essential to this process.
By serving as an essential middleman and ensuring that claims are correctly prepared, verified, and sent to insurance payers, clearinghouse claims submission provides a simplified answer to these problems. Clearinghouses help make the claims process easier and more productive by combining cutting-edge technology and industry knowledge, which eventually benefits patients and providers.
What is a Clearinghouse Claims Submission in Healthcare?
In the healthcare industry, a clearinghouse refers to an outside organization that oversees the electronic submission of medical claims to insurance payers. Before sending claims to the relevant payers, they make sure the formatting is accurate and complies with industry standards.
The Significance of Clearinghouses
Clearinghouse claims submission expedite the billing process, lower the rate of claim submission errors, and speed up reimbursement. In order to prevent claim rejections or delays, they serve as an essential checkpoint.
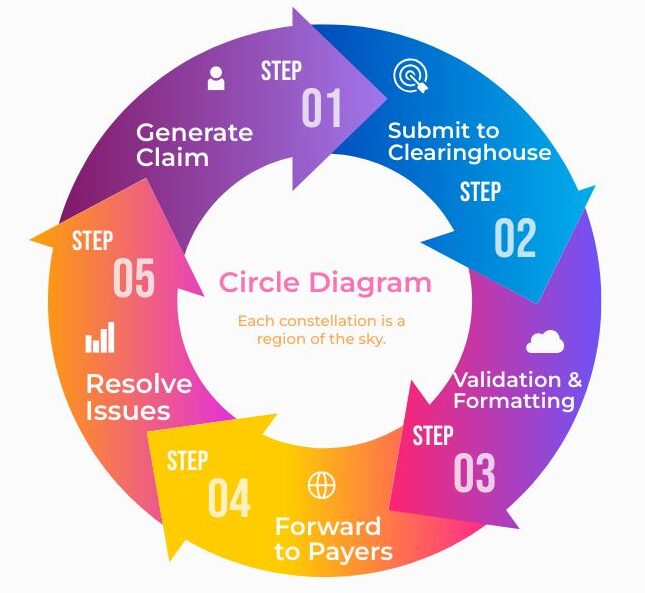
The Process of Submitting Claims to the Clearinghouse
Step 1: Getting the Claim Ready
Healthcare providers are required to collect all relevant patient data, such as insurance information, personal information, and service codes (CPT, ICD-10), prior to filing a claim. At this point, accuracy is essential to preventing claim rejections.
Step 2: The Clearinghouse is consulted
The claim is prepared and then electronically sent to the clearinghouse. As part of this submission, the data is frequently transformed into an ANSI X12 or other standardized format, which is necessary for electronic data interchange (EDI).
Step 3: Cleaning Up Claims
According to a procedure known as “claim scrubbing,” clearinghouses examine claims for mistakes or discrepancies. This entails verifying patient data, making sure that the right codes are being used, and making sure that payer-specific guidelines are being followed.
Step 4: Sending to Recipients
The claim is cleaned up and then sent to the right insurance payers. Errors found by the clearinghouse are reported back to the provider so they can be fixed before resubmitting the claim.
Step 5: Monitoring and Acknowledgment
Clearinghouse claims submission help providers stay informed about the status of their claims and any necessary actions by offering tracking for submitted claims and acknowledgment receipts.
Advantages of Using a Clearinghouse:
- Increased Precision
By lowering the possibility of mistakes, clearinghouses guarantee that claims are correct and comprehensive before they are sent to payers.
- Accelerated Payment
Clearinghouse claim submission facilitate faster payment receipts for healthcare providers by reducing errors and optimizing the submission process.
- Savings on Costs
Lowering rework and claim denials can greatly cut down on billing administration expenses.
- Improved Occupancy
Clearinghouse claim submission assist providers in adhering to industry regulations by guaranteeing that claims fulfill regulatory standards.
Clearinghouse claims submission simplifies healthcare billing.
How to Select the Best Clearinghouse:
Important Considerations
A clearinghouse claims submission should be chosen after taking into account various aspects like price, customer service, ease of integration with current systems, and services provided.
Connectivity to Software for Practice Management
Reducing manual data entry and streamlining the billing process can be achieved by selecting a clearinghouse that works seamlessly with your practice management software.
Assistance to Customers and Education
It’s imperative to have competent customer service and training, particularly when working with intricate billing systems and regular changes to healthcare regulations.
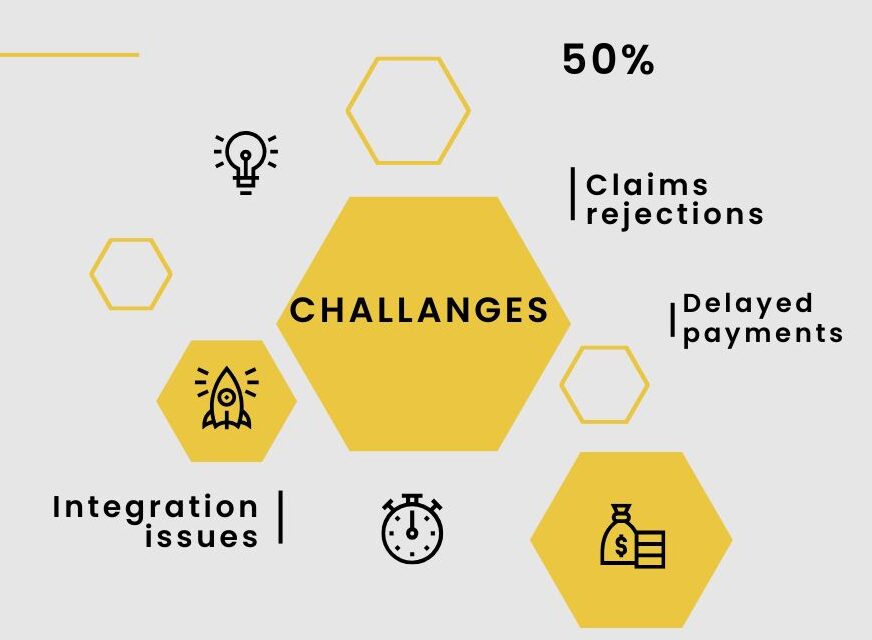
Typical Obstacles in Claims Processing
- Entry Errors in Submission Data
Errors in data entry, like coding mistakes or inaccurate patient information, may result in the denial of claims.
- Issues with Compatibility
Processing of claims may be hampered by delays and inaccuracies due to system compatibility problems between the clearinghouse and the healthcare provider.
- Observance of Regulatory Modifications
It is crucial to stay informed about modifications to insurance requirements and billing codes in order to prevent denials and guarantee compliance.
The Best Ways to Maximize the Use of Clearinghouse Claims Submission
Update Your Coding Knowledge Often
Accurate clearinghouse claims submissions depend on staying up to date with coding changes, such as updates to CPT, ICD-10, and HCPCS codes.
Perform Audits on a Regular Basis
Frequent reviews of claims that have been submitted can aid in spotting trends in denials or rejections, enabling specific enhancements to the submission procedure.
Instruction and Training
Accuracy and overall efficiency can be increased by providing billing staff with ongoing education and training on the most recent software updates and industry standards.
| Step | Description |
| Claim Preparation | Gathering patient and service information. |
| Claim Submission | Sending the claim electronically to the clearinghouse. |
| Claim Scrubbing | Reviewing the claim for errors and compliance. |
| Forwarding to Payers | Sending the clean claim to insurance payers. |
| Acknowledgment | Receiving confirmation of claim receipt. |
| Tracking | Monitoring the status of the claim and resolving issues. |
The Importance of Clearinghouse Claims submission in Medical Billing
In the healthcare billing process, clearinghouses play a crucial role as a liaison between insurance payers and healthcare providers.
Streamlining the submission of insurance claims is their main responsibility, along with making sure that they are accurate, correctly formatted, and adhere to payer-specific requirements as well as industry standards.
This function plays a critical role in reducing errors and enabling prompt reimbursement for provided services.
Improving the Correctness of Clearinghouse Claim Submission
Improved claim submission accuracy is one of the biggest advantages of using a clearinghouse. Complex coding systems, including CPT, ICD-10, and HCPCS codes, are used in healthcare billing; proper use is essential to prevent claim denials.
Advanced software is used by clearinghouses to check for common errors like missing data, invalid codes, and inaccurate patient information.
By ensuring that only clear, error-free claims are sent to insurance payers, this “claim scrubbing” procedure greatly lowers the possibility of claims being rejected or denied.
Choose the right clearinghouse for your practice
Making Billing More Efficient
Since it has a direct impact on cash flow and financial stability, billing process efficiency is crucial for healthcare providers.
Reducing the need for manual entry and paperwork, clearinghouse claims submission automate the submission of claims, streamlining the process.
Billing employees can now concentrate on other crucial duties, like following up on unpaid claims and answering patient inquiries, as this automation expedites the submission process. This leads to faster reimbursement turnaround times and an overall more efficient operation.
Minimizing Expenses of Administration
In the medical field, administrative expenses can add up, especially when it comes to billing and filing claims.
Clearinghouse Claims submission mistakes can result in a large amount of rework, such as dealing with payer denials and resubmitting amended claims. Providers can lower these expenses by utilizing a clearinghouse to minimize errors.
Moreover, clearinghouses frequently offer analytics and tools to help find and fix problems in the billing process, which results in long-term savings and enhanced financial performance.
Encouraging Improved Payer Communication
Additionally, clearinghouse claims submission facilitate communication between insurance payers and healthcare providers.
They offer thorough reports and acknowledgments that enable providers to monitor the progress of their claims and spot any problems that require attention.
This openness in the claim’s procedure facilitates quicker resolution of any disagreements or inconsistencies that may emerge and enhances communication with payers.
Enhancing Management of the Revenue Cycle
Strong revenue cycle management (RCM) is critical to any healthcare provider’s bottom line. By ensuring that claims are processed accurately and quickly, clearinghouses are essential to optimizing RCM.
Clearinghouse claims submission assist providers in preserving a consistent cash flow and shortening the time it takes to collect payments by decreasing errors and expediting the reimbursement process.
Providers are able to make investments in patient care and staff development as well as other aspects of their practice because of their increased financial stability.
Key Benefits and Functions of Clearinghouses in Healthcare Billing
- Clearinghouse claims submission act as a middleman between insurance companies and healthcare practitioners.
- They support the accuracy and adherence to industry standards of insurance claims.
- Clearinghouses do “claim scrubbing” to make sure there are no mistakes or discrepancies.
- They reduce manual data entry and paperwork by streamlining the claims submission process.
- Healthcare providers may receive their payments more quickly if they use a clearinghouse.
- Clearinghouse claims submission aid in the reduction of rework and billing error-related administrative expenses.
- They guarantee adherence to laws like HIPAA, safeguarding patient information.
- Analytics and tools are offered by clearinghouses to enhance the billing procedure.
- They help insurance payers and providers communicate more effectively.
- Better revenue cycle management is a result of clearinghouse utilization done well.
In summary
Clearinghouse claims submission is essential to the healthcare billing ecosystem because it serves as a crucial middleman and improves the speed and precision of the claim’s procedure. Clearinghouses greatly minimize the possibility of errors, accelerate reimbursement processes, and assist in efficiently managing administrative expenses by optimizing the submission workflow.
Their significance for preserving a robust revenue cycle is further highlighted by their capacity to guarantee adherence to industry rules and promote efficient communication between healthcare providers and insurance payers.
Clearinghouses play an increasingly important role in streamlining and optimizing claims submission as the healthcare industry continues to change due to new regulations and technological advancements.
Healthcare providers can focus on providing high-quality patient care while maintaining financial stability by utilizing a clearinghouse’s capabilities.
Taking advantage of clearinghouse services can result in improved cash flow, streamlined billing procedures, and more effective operations, all of which can boost the long-term viability and success of medical practices.
FAQs
How do I select the appropriate clearinghouse?
Think about the size of your practice, your unique requirements, and the features offered by the clearinghouse, like real-time tracking and support.
What are the benefits of submitting claims through a clearinghouse?
By using a clearinghouse, you can expedite processing, lower error rates, and guarantee that claims satisfy payer requirements.
Does using a clearinghouse come with any costs?
Yes, clearinghouses usually charge for their services; the cost will depend on the volume and features of the clearinghouse.

